Acute rhinosinusitis is diagnosed when the patient has acute symptoms (purulent nasal drainage accompanied by nasal obstruction, facial pain, or a sense of pressure, fullness, or both) for up to 4 weeks. The acute form can be, depending on the responsible agent, bacterial or viral; recurrent if present more than four times a year in the absence of intermediate symptoms. Between one episode and the next. Here we will give you a complete guide about antibiotics for sinus infection.
Suppose acute symptoms (purulent nasal drainage accompanied by nasal obstruction. Facial pain, or a sense of pressure, fullness, or both) persist without improvement. For at least 10 days beyond their onset or worsen within 10 days. Additional signs and symptoms of the bacterial form include fever, cough, fatigue (malaise), reduced (hypos my), or missing (anosmia). Sense of smell, jaw dental pain, and a sense of fullness or intra-auricular pressure.
What is a sinus infection?
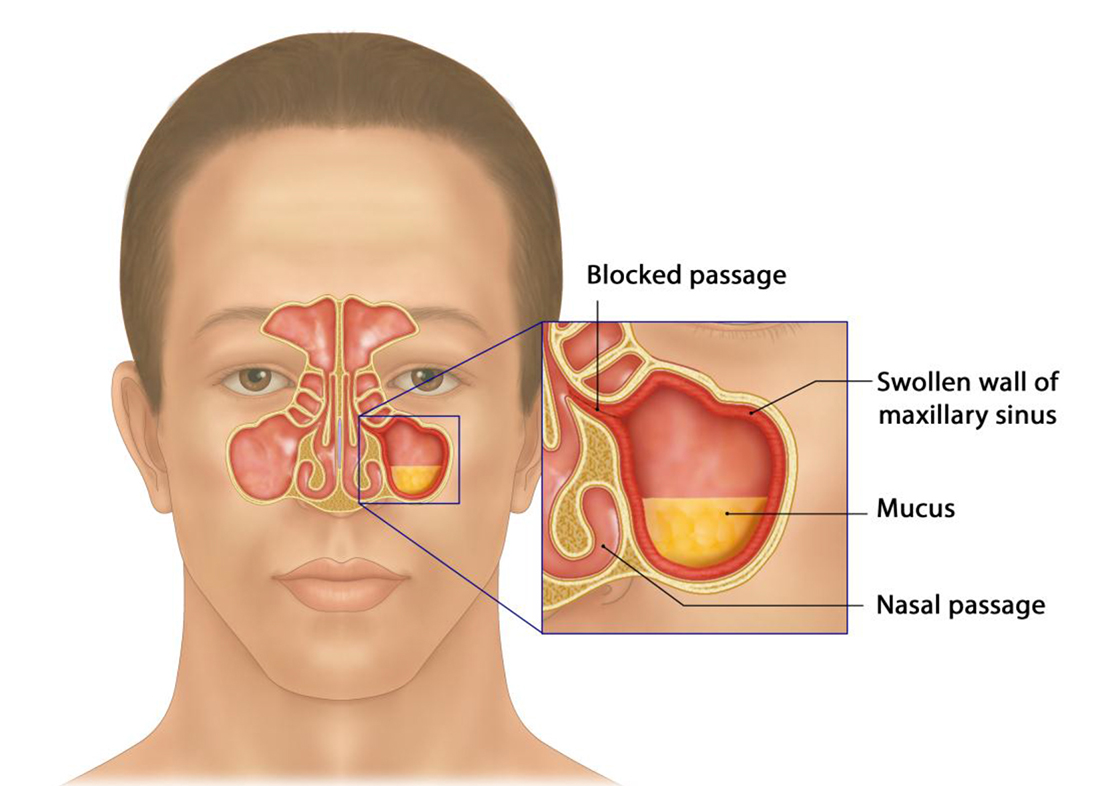
Often confused with the common cold due to symptoms very similar to each other. Sinusitis is a state of inflammation of the mucous membranes located below the facial sinuses. Usually caused by bacteria, more rarely by viruses and fungi (for example, in some people with a weakened immune system or allergic individuals).
In general, we speak of rhinosinusitis because the nasal cavities system and the paranasal sinuses constitute a single system. Among the conditions favoring the onset of sinusitis. The conditions of the meatal ostium complexe are the passage and drainage point. Between sinus cavities and paranasal sinuses, which favors the process’s establishment. We can have anatomical conditions that alter the passage of air currents inside the nose or functional factors. Such as allergic rhinopathy or cellular rhinitis (NARES, NARS). Which due to the presence of certain cells in the nose. Such as mast cells and/or eosinophils and the factors. That release determines a state of chronic imbibition of the tissues that hinders drainage, leading to polyposis. And sinus stagnation, which will then turn into sinusitis. There may rarely be a congenital disability of ciliary motility.
Subacute if it lasts for about 1-3 months, chronic if it lasts longer. When a person is suffering from sinusitis. The mucous membranes swell, and mucus remains trapped within the sinuses themselves and assumes greater features. It has a greenish-yellow color becoming frankly purulent. This accumulation of mucus in the ideal prerequisite for the reproduction of fungi and bacteria.
Sinus infection Kinds: Antibiotics For Sinus Infection
Sinusitis is classified according to different characteristics. There is an acute form (less than 3 months) and chronic (more than 3 months). If the disease in an acute form recurs several times a year, they talk about recurrent sinusitis. Chronic sinus inflammation has varying degrees of morphological changes and can be catarrhal, purulent, polyposis, allergic, necrotic; there are other, more rare, options.
An exacerbation of chronic sinusitis is understood as adding new symptoms and/or increasing existing ones’ severity. Distinguish between mild, moderate, and severe sinusitis. Depending on the affected sinus, there is sinusitis, frontal sinusitis, ethmoiditis, sphenoids, or their combination.
Depending on the causative agent of the pathology, such variants of sinusitis are distinguished:
- viral, caused by adeno, rhinos, coronaviruses, influenza virus, parainfluenza, respiratory syncytial, and other causes of ARVI;
- bacterial, caused most often by pneumococcus, Moraxella, or Haemophilus influenza; among this group, sinusitis is distinguished against the background of immunodeficiencies, nosocomial (developed during a hospital stay), odontogenic (associated with dental diseases);
- It often occurs with prolonged irrational treatment with antibiotics or damage by highly pathogenic fungi, including systemic mycoses.
Treatment of sinus inflammation is carried out, taking into account the duration, severity of the disease, and its causative agent.
Diagnosis
Radiographic examinations are not indicated in suspicion of acute rhinosinusitis unless it is a complication. An alternative diagnosis is suspected based on severe headache, facial tumefaction, cranial nerve palsy, or eyeball displacement (proptosis ). The presence of a fluid level and moderate or severe thickening of the mucosa. Analgesic drugs, topical intranasal steroids and/or nasal washes for relief, decongestants, mucolytics, cough sedatives are indicated. Pain relief is the goal, often the reason that brings the patient to the doctor’s attention.
For this purpose, topical nasal steroids have been used alone or combined with oral antibiotics. And nasal washings can improve the course, decreasing symptoms, particularly in patients with frequent episodes. More than 3-5 consecutive days to avoid reactive withdrawal congestion and drug rhinitis.
Initial therapy of acute bacterial sinusitis
Watchful waiting should only be offered when the patient is under close clinical supervision to initiate antibiotic therapy promptly. The condition does not improve within 7 days of diagnosis, or if it worsens at any time. In fact, it is appropriate not to prescribe antibiotics in the initial management and with the only clinical diagnosis. Because many patients will improve spontaneously. In fact, it is permissible to wait up to 7 days after diagnosis, limiting itself. To symptomatic relief before administering antibiotics.
To eradicate the bacterial infection from the sinuses, accelerate symptom resolution, and improve symptoms.
For patients allergic to penicillin, both doxycycline and fluoroquinolone (levofloxacin or moxifloxacin) are recommended, again for up to 10 days. Macrolide antibiotics and trimethoprim-sulfamethoxazole are not indicated for the initial therapy of bacterial forms.
Acute bacterial sinusitis therapy in case of initial failure
Suppose the patient fails to improve within 7 days of diagnosis or worsens during initial management. If you have opted for watchful waiting at this point, it would be advisable to initiate antibiotic therapy. It would be appropriate at this point to change. The 7-day wait helps define initial treatment failure and helps avoid unnecessary medication or inadequate diagnostic tests.
High-dose amoxicillin with clavulanate, doxycycline, or a respiratory fluoroquinolone (levofloxacin or moxifloxacin). Suppose the patient worsens or does not improve after 7 days of the new therapy. It is advisable to evaluate the possibility of an infection with drug-resistant bacteria and then investigated with an antibiogram.
Also Read: Low Blood Pressure Symptoms
Chronic rhinosinusitis
It is primarily an inflammatory disease, with occasional exacerbations associated with infection. Nasal polyps and, as mentioned, recurrent acute episodes may be present. Symptoms vary in severity and presentation: nasal obstruction is the most common (81% -95%). She was followed by a feeling of congestion-pressure-fullness of the face (70% -85%), purulent nasal discharge (51% -83 %). Hyposmia (61% -69%), headache, fever, cough, bad breath, fatigue, and dental pain. And other non-specific signs or symptoms.
The presence of 2 or more signs or symptoms. That persists beyond 12 weeks indicates chronic rhino-sinusitis diagnosis. In addition to the clinical symptoms. With particular attention to the middle turbinate: CT imaging is the standard diagnostic criterion.
Differential diagnostics include allergic rhinitis, non-allergic rhinitis, vasomotor rhinitis, eosinophilic non-allergic rhinitis, sept nasal deformity. And non-rhino genic causes of facial pain (neurological disorders such as vascular headaches, migraine, cluster headache, trigeminal neuralgia, temporal disorders -mandibular). Treating only episodic infections while leaving the underlying condition untreated contributes to a higher frequency of exacerbations. Bacterial infection can more easily persist with nasal sinus obstruction related to edema and mucus trapped in the sinuses.
Diagnosis
It is always necessary to confirm the clinical diagnosis with instrumental documentation on the nasal sinus inflammation by anterior rhinoscopy, nasal endoscopy, or CT scan. Objective confirmation of Sinonasal inflammation done by direct visualization or by CT scan.
How to prevent sinus infection: Antibiotics For Sinus Infection
The prevention of sinusitis is fundamentally based on the treatment of allergies (many allergy sufferers are subject to sinusitis). They stay in temperatures too hot or too cold or too dry to avoid contact with pollutants.
The use of decongestants in upper respiratory infections can reduce the risk of sinusitis.
Also Read: Symptoms Of Strep Throat
Sinusitis therapy
The goals of treatment are to cure the underlying infection and improve symptoms. The antibiotics are the treatment of bacterial sinusitis, associated with nasal lavage and local medical therapy. The therapy must always be completed without interrupting it as soon as improvements are noticed. Otherwise, the treatment will not affect. Indeed it could induce antibiotic resistance in the patient.
To relieve symptoms, the use of decongestants and mucolytics can help clear the sinuses of excess mucus. If antibiotic therapy does not give the desired results, it may be necessary to resort to surgery. The operation promises to be the only therapy for those with nasal defects. Such as the deviation of the septum or the presence of polyps. But also in the case of sinusitis of fungal origin.
Symptomatic therapy of chronic sinusitis
Nasal irrigation with saline solution. The improvement of mucosal clearance and increased ciliary activity allows removing antigens, biofilm, and inflammatory mediators. That directly protects the nose mucosa -sinusal.
Surgical therapy
Functional endoscopic sinus surgery aims to enlarge—the most-meatal unit’s restricted areas (the communication between the sinus and the nasal cavity). At the same time, we are preserving the marginal mucosa guaranteeing ventilation and drainage of the affected paranasal sinuses.
This helps restore the mucociliary activity that removes the factors responsible for inflammation, thanks to topical intranasal therapy’s greater effectiveness. And under local anesthesia with anterior intraoral or intranasal accesses.
Drug therapy
The mainstay of treatment for sinus inflammation is antibiotics. Amoxicillin, amoxicillin-clavulanate, cephalosporins, macrolides, fluoroquinolones are used.
Additional medications for sinusitis: Antibiotics For Sinus Infection
- decongestants in the form of drops or nasal sprays lasting no more than five days; these drugs constrict blood vessels, relieve mucosal edema, and create conditions for the outflow of pathological contents of the sinus;
- They dry the mucous membrane and reduce swelling;
- pain relievers, such as NSAIDs
- local use of antiseptics (rinsing the nose with furatsilin solution), irrigation therapy (Miramistin, Squalor, Dolphin, means based on seawater or saline solution with the addition of iodine);
- in chronic sinusitis (except for the odontogenic variant), the course use of glucocorticoid-based sprays, which suppress inflammation, is acceptable; a doctor should prescribe them.
Traditional medicine
Such recipes help to improve nasal breathing, relieve inflammation and edema, and strengthen local immunity. The following remedies can help:
- inhalation based on chopped garlic mixed with apple cider vinegar;
- the introduction of tampons soaked in a mixture of onion juice, honey, and sunflower oil into the nose;
- instillation of aloe juice, radish, onion, a variety of beetroot juice and honey, propolis into the nose;
- compresses on the area of the affected sinus with a decoction of calendula, plantain, chamomile.
Operation: Antibiotics For Sinus Infection
Such a surgical intervention as a puncture of the affected sinus with the removal of pus and washing. Which is often accompanied by complications (damage to the orbit, upper jaw, air embolism, and others). Both traditional with open surgery on the sinuses and minimally invasive with the use of endoscopic techniques:
- interventions aimed at eliminating anatomical deformities – septoplasty, removal of adenoids and others;
- intranasal antrostomy – creating a hole in the wall of the maxillary sinus into the nasal cavity;
- radical antrostomy – producing a permanent drainage hole by removing part of the bony wall of the sinus.
Also Read: A Healthy Spine with Chiropractic Care for Back Pain Relief










